Bioinspired robotic exoskeleton for endotracheal intubation
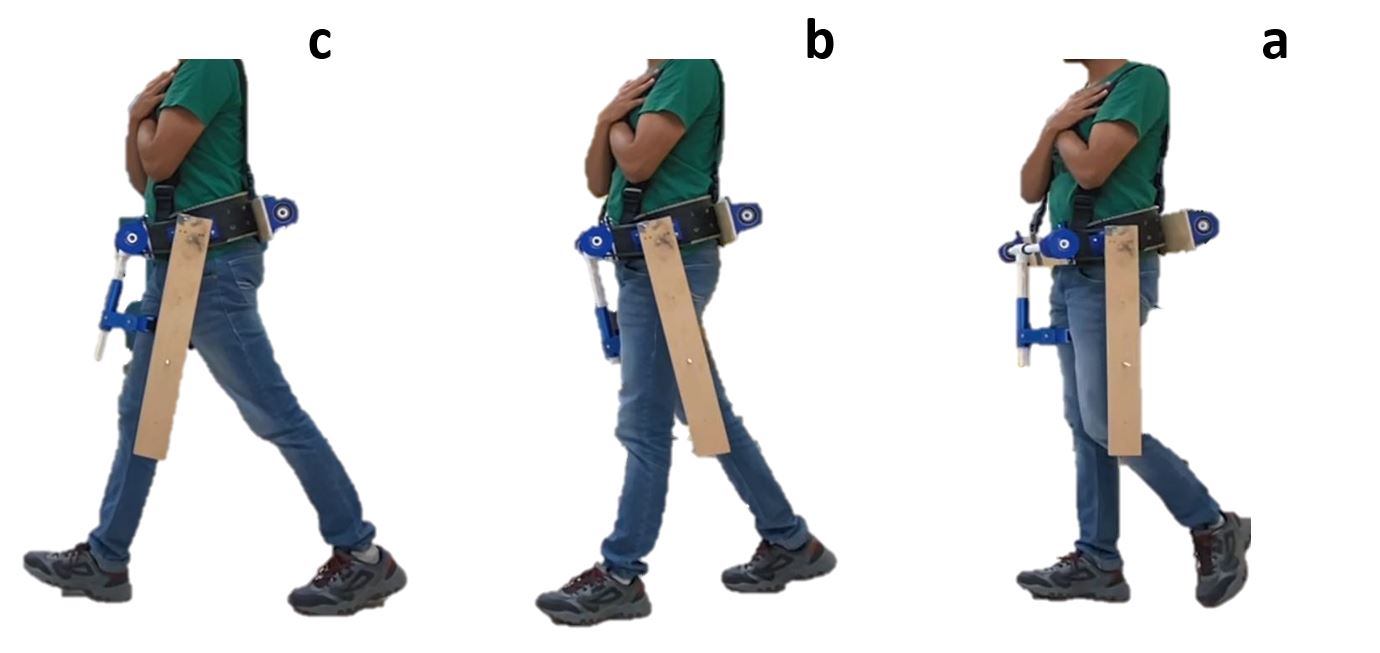
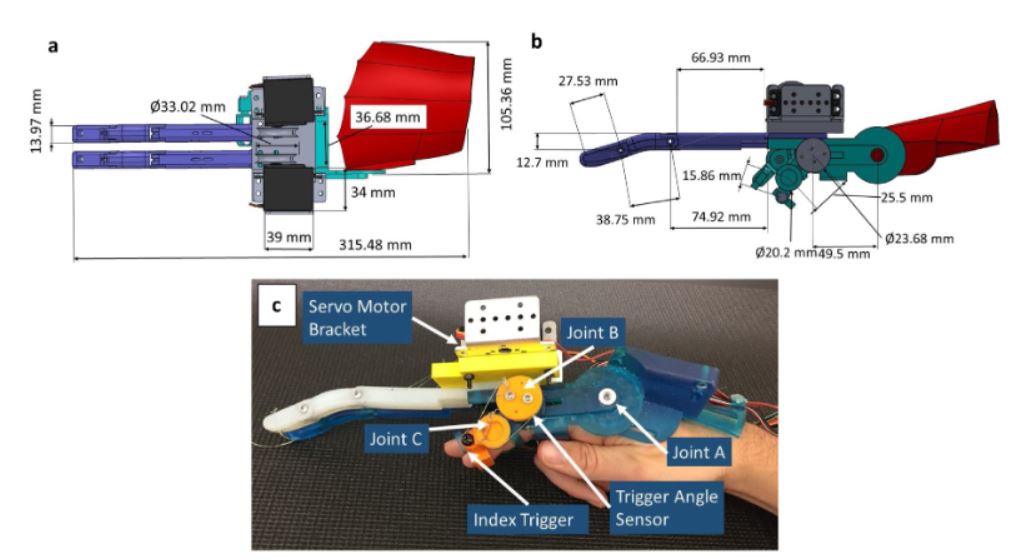
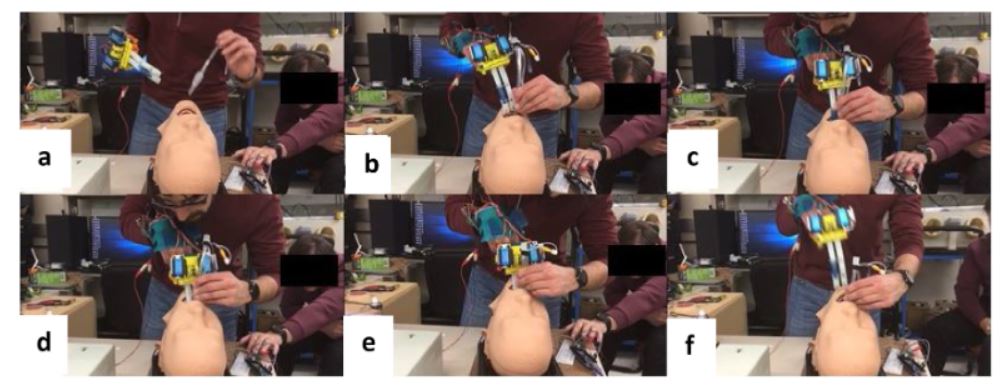
Airway management is a priority to any caregiver in a trauma scenario. The current clinical gold standard for airway securement is endotracheal intubation (ETI), which involves placement of an endotracheal tube into patient tracheas and pneumatically expanding a cuff for securement. Incorrect performance of this delicate and complex procedure poses significant risks to patients, as excessive force and leverage during insertion can damage sensitive airway tissues, especially when performed by less-skilled providers or executed in difficult airway situations. The present study investigated the development of a bioin- spired mechanical platform termed the Digital Extenders, which is capable of augmenting a provider’s reach for ETI. A prototype that could apply an output force of at least 20 N was designed for comparative analysis versus current clinical approaches. Performance analysis studies utilized an innovative instrumented mannequin model to compare force employed during intubation with the Digital Extenders versus direct laryngoscopy and digital intubation. Resulting data showed that there is an important reduction in applied force at the base of the tongue using the novel Digital Extenders platform; such a reduction of applied force is important in enabling the provider to secure the airway, causing less trauma to the patient. In addition, the use of the Digital Extender protects the provider’s digits from patient bite reactions typical from intubation when the patient is not sufficiently sedated. These study results motivate continued development of the Digital Extenders as a less traumatic approach to ETI. Future consideration may investigate challenges in mannequins’ biomimicry of physiological properties.
Conclusion
Overall, the present study demonstrated the successful initial prototyping and characterization of an innovative, bioinspired DEs mechanical platform that can augment a provider’s reach for ETI. Furthermore, the study utilized a novel instrumented mannequin model to compare intubation with the novel device versus current clinical standards of direct laryngoscopy and digital intubation. The data supports the hypothesis that the DEs platform can reduce the applied force for intubation, thereby presenting a promising path toward developing a less traumatic option for airway management. One conclusion counter to a study hypothesis was that the DEs platform did not reduce the head/neck movement relative to other methods of ETI. Envisioned future enhancements to the design of the DEs will incorporate haptic feedback to provide phantom sensation for the provider from the distal tips of the DEs.